History
Combined excellence in research, training and clinical service since 1910
The Department of Pathology & Immunology’s three-part mission to advance research, training and clinical service has continued to strengthen over the years and act as a bridge between the basic and clinical sides of medicine across the university. Today, the department is considered one of seven basic science departments of the School of Medicine, with a strong emphasis on immunology.

The department has had 10 heads since the reorganization of the medical school following the Flexner report in 1891, a comprehensive study of medical education that emphasized a focus on higher educational standards and a dedication to mainstream science.
- Eugene Opie, MD, led the department from 1910 to 1923. Dr. Opie was a prominent experimentalist, the first to describe the pathology of diabetes and to carry out extensive analysis of the tuberculous granuloma. He served as dean of the School of Medicine from 1912 to 1915.
- Leo Loeb, MD, (1923-1938) cultivated the very close association of pathology with immunology and biomedical research. He was one of the first investigators to study the relationship between self and non-self by using tissue transplantation. He also made important contributions in areas of endocrinology and cancer research.
- Howard McCordock, MD, (1938-1939), an excellent anatomic pathologist and teacher, died suddenly of complications of rheumatic fever soon after assuming leadership of the department.
- Robert Moore, MD, (1939-1954) provided an administrative and clinical focus to the department and helped bring it into the contemporary era. He served as dean of the medical school from 1946-1954.
- Stanley Hartroft, MD, PhD, (1954-1961) a scientist with interests in liver disease, restored the department’s strong emphasis on research.
- Paul Lacy, MD, PhD (1961-1985) pioneered the development of procedures for isolating pancreatic islets, as well as the use of islet cell transplantation for the treatment of diabetes.
- Emil Unanue, MD, (1985-2006) arrived from Harvard in 1985, already recognized for seminal contributions relating to antigen presentation. He established the vigorous immunology program and created the integrated Department of Pathology and Immunology.
- Herbert (Skip) Virgin, MD, PhD, (2006-2017) focuses his research on the immune response to chronic viral infections.
- Charles S. Eby, MD, (2017-2019) became interim head following Virgin. His research focuses on the genetic contribution to the variability of warfarin dosing.
- Richard Cote, MD, (2019-2025) a physician-scientist and entrepreneur specializing in cancer, was named head of the department in 2019.
- Eric Huang, MD, PhD, (2025-Present) a physician-scientist renowned for expertise in human brain development and degeneration.
History of clinical labs at Barnes Hospital
We have a long and rich history of contributions to diagnostic pathology and patient care. The modern era of surgical pathology began with the arrival of Lauren V. Ackerman, MD, at Barnes Hospital in 1948.
Prior to this time, anatomic pathology was divided along traditional lines; academic efforts in pathology were based on post-mortem investigations or bench science, while surgical pathology was performed by surgeons. The appointment of Dr. Ackerman, who was not a surgeon, signaled formal recognition that surgical pathology had matured to become a bona fide clinical discipline.
By the early 1960s, surgical pathology had become an integral part of the Department of Pathology. Dr. Ackerman’s trainees and those who followed have propagated his influence, here and abroad, and shaped surgical pathology as a clinical discipline.
Timeline
Before the Division of Laboratory and Genomic Medicine was formed, faculty from the Department of Medicine directed the clinical laboratories at Barnes Hospital on a part-time basis. Virgil Loeb, Jr., MD, from the Divisions of Hematology and Oncology served as Director of Barnes Hospital laboratories from 1953 to 1969. William Daughaday, MD, Metabolism Division Director and an internationally known endocrinologist who discovered insulin-like growth factor I, served as a consultant for the chemical and endocrine laboratories.
In 1969 the Division of Laboratory Medicine was founded as a co-division of the Departments of Medicine and Pathology. Thanks to the increasing volume of testing, complex new automation and quality assurance and maintenance requirements, the clinical laboratories required full-time oversight. The two departments also envisioned an academic division where faculty could participate in research, train residents in clinical pathology and provide medical direction to the clinical laboratories at Barnes Hospital.
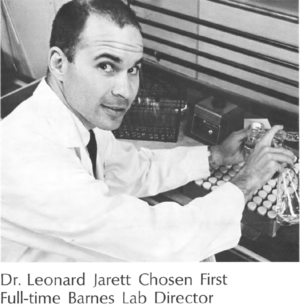
The first director of the division was 32-year-old Assistant Professor of Pathology, Leonard Jarett, MD. Dr. Jarett graduated from Washington University School of Medicine in 1962 and went on to complete his internship in internal medicine and residency in pathology at the School of Medicine. Section chief consultants were William Daughaday, MD, (clinical chemistry), Carl Harford, MD, (clinical microbiology), Charles Parker, MD, (allergy) and Virgil Loeb, MD, (hematology, blood bank and clinical microscopy). Among the challenges facing Dr. Jarett at the time were expansion, relocation and reorganization of the clinical laboratories and concurrent expansion of the division’s academic mission.
The first move Jarett oversaw was consolidating clinical chemistry, clinical hematology and clinical immunology and the blood bank into one general area on the second floor of Barnes Hospital in 1970. Clinical hematology and microbiology remained in this area until 2016.
The installation of a Technicon instrument that could run 18 chemistry tests in 10 minutes also marked Barnes Laboratory as the first in St. Louis, and one of the first in the country, to use this fully automated chemistry analyzer (shown below).

Another major accomplishment of the division was installing the first laboratory information system (LIS) in the St. Louis area in 1972, to connect laboratory instruments to a computer system that contained patient registration information and laboratory results. This system allowed patient results to be retrieved instantly with a phone call to the lab and a printed cumulative report for every patient’s laboratory results on a nightly basis.
Between 1972 and 1976, the clinical pathology residency, clinical chemistry fellowship and transfusion medicine fellowship programs began, leading to the rapid expansion of faculty in the division.
By 1972, clinical chemistry testing volume was continuing to increase due to automation, as well as the addition of many new testing methods including chromatography, ion-specific electrodes, immunoassays and electrophoresis.
Jack Ladenson, PhD also joined the clinical chemistry section that year (he remains a part-time member of the faculty in the division). His research focused on calcium ion-specific electrodes. One of his first major clinical contributions was using the new LIS to develop a “delta system,” which used a patient as their own control. When a patient result changed beyond normal physiologic variability the result would “delta” against a prior result and help identify laboratory or pre-laboratory error.
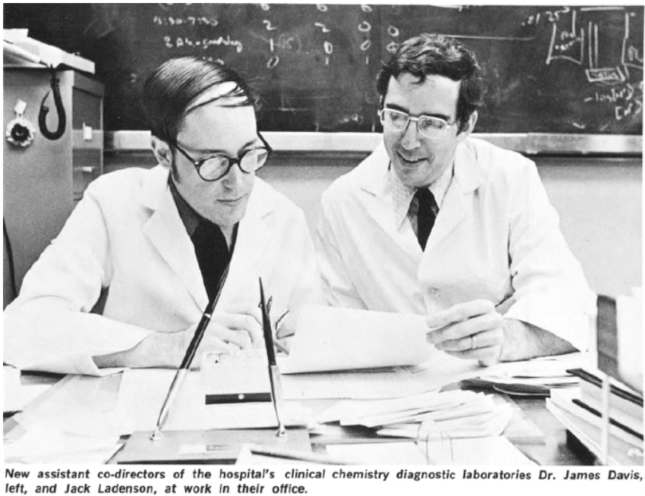
In 1976, Jay McDonald, MD joined Dr. Ladenson as co-director of clinical chemistry. Dr. McDonald came to the School of Medicine after completing a pathology residency at Wayne State University in 1974. He was a postdoc in Dr. Jarett’s research lab, and he also completed a clinical chemistry fellowship under Dr. Ladenson’s tutelage. Dr. McDonald’s research interest revolved around the role of calcium signaling in insulin activity.
Throughout the 1970s, under Dr. Jarett’s guidance, the division became a national leader in academic laboratory medicine with a strong clinical pathology residency, diverse research activities and strong clinical service to the hospital. Faculty thrived and grew as “triple threats” with excellent research, teaching and clinical skills.
The 1980s were a decade of change, growth and scientific accomplishment for the division. In 1980, when Dr. Jarett was named Chair of the Department of Pathology at the University of Pennsylvania (where he remained until his retirement in 2000), Jay McDonald, MD was named Division Chief. During this time, faculty became employees of the medical school rather than Barnes Hospital. Salary support for faculty clinical responsibilities under Medicare Part A was negotiated in a contract with the hospital that remains the model for the relationship of division faculty with Barnes-Jewish Hospital to this day.
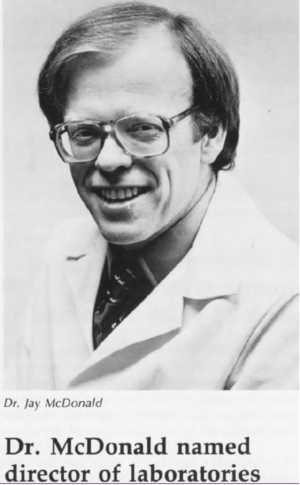
Dr. McDonald expanded the residency program and continued to increase the number of division faculty. The weekly Friday morning Lab Medicine Rounds conference became known as the “shark tank,” as Dr. McDonald was a strong critical evaluator of the clinical content of resident presentations.
Some key faculty members joined the division at this time:
- Doug Lublin, MD, PhD – paroxysmal nocturnal hematuria
- Sam Santoro, MD, PhD – alpha2-beta 1 integrin-mediated cell adhesion
- Joe Miletich, MD, PhD – protein C deficiency and thrombosis
- John Turk, MD – diabetes
- Moon Nahm, MD – immune response to bacterial carbohydrates.
In 1986, Dr. Ladenson discovered and patented the first monoclonal antibodies specific for Creatine kinase-MB (CK-MB), which were licensed and used in every commercial CK-MB immunoassay for many years and revolutionized rapid detection of acute myocardial infarction.
In 1990, Dr. McDonald was named Chair of Pathology at the University of Alabama Birmingham where he finished his career in 2014. In 1991, Joe Miletich, MD, PhD was named Division Chief and led the division through expansions of faculty and services.

In 1993, Barnes Hospital and its neighbor, Jewish Hospital, merged to become Barnes-Jewish Hospital. Clinical laboratory services for the two hospitals were consolidated under the division’s direction and Jewish Hospital laboratory medical directors became members of the division. This merger was the first step in the formation of the 14 hospital Barnes-Jewish-Christian (BJC) Healthcare network in 1996.
Despite the formation of this large healthcare network, the division’s clinical responsibilities remained solely with Barnes-Jewish Hospital and would remain so for the next 20 years.
In 1990, the human genome project began and division members were involved from the very beginning. Washington University was one of only a handful of main sites for the project and clinical pathology resident, later faculty member, and current Director of the National Human Genome Research Institute, Eric Green, MD, PhD was instrumental in determining the entire sequence of human chromosome 7.
In line with the expansion of nucleic acid technology that began in the 1990s, the division’s first molecular diagnostics laboratory was established under the initial direction of Jeff Milbrandt, MD, PhD and later Barbara Zehnbauer, PhD, who joined the division as Medical Director of the Molecular Diagnostics Lab.
Having already established his place in division history, Dr. Ladenson made another seminal discovery, describing the first monoclonal antibodies-based immunoassay for cardiac troponin I (cTnI) in 1992. Like his antibodies to CK-MB, these cTnI-specific antibodies became the basis of the first commercial assays for the diagnosis of acute myocardial infarction.
In the late 1990s, Dr. Ladenson began using some of the income from his inventions to help develop laboratory medicine in developing nations. The division became the reference lab and source of quality control oversight for the entire African nation of Eritrea through the 2000s, and supported laboratory medicine in developing countries such as Bhutan, Haiti, Namibia, Ghana, Ethiopia and others.
In 2000, Dr. Miletich became Senior Vice President of Pre-clinical Affairs at Merck, and Sam Santoro, MD, PhD, former resident and division faculty since 1982, was named Division Chief. Dr. Santoro kept the division moving forward, championing the three-pronged mission of research, clinical service and training. He strongly supported faculty involvement in national organizations and increased the division’s national and international visibility.
Initiatives under Dr. Santoro included beginning new fellowships in clinical microbiology and molecular diagnostics. The division support of clinical laboratories in developing nations gained full momentum, with Dr. Ladenson backing multiple faculty and trainees who would visit these laboratories to help them standardize and modernize.

In 2003, Dr. Santoro was named Chair of Pathology at Vanderbilt and Dr. Ladenson served as Interim Division Chief until 2007.
Jeffery Gordon, MD, PhD joined the division during this time as Director of the Edison Family Center for Genome Sciences and Systems Biology. Dr. Gordon is often referred to as the “father” of gut microbiome research and has received numerous honors such as the Louisa Gross Horwitz Prize, the Copley Medal from the Royal Society in Britain and the Sanofi-Institut Pasteur International Award that recognize his role in this field.
In 2006, the name of the division was changed from Laboratory Medicine to Laboratory and Genomic Medicine to reflect the increasing role of molecular diagnostics and personalized medicine for the oncology and other services at Washington University.

In 2007, Barry Sleckman, MD was named Division Chief and almost immediately began expanding the research track faculty within the division. The number of primary faculty increased from 22 in 2006 to 37 today as a result of the recruitment of talented researchers by Dr. Sleckman.
In 2009, the Genomics and Pathology Services (GPS) began. A joint effort between the Department of Genetics and Pathology and Immunology, GPS provides physicians with clinically validated next-generation sequencing for cancer and a variety of constitutional diseases.
The most significant educational initiatives during Dr. Sleckman’s leadership included revision of the clinical pathology (CP) training curriculum to reflect the growing role of molecular diagnostics and establishment the Physician Scientist Training Program (PSTP) for clinical pathology residents. The PSTP program identifies several CP residents every year who, following residency, receive three years of postdoctoral research support in order to establish themselves as solid researchers. The program has proven to be enormously successful and continues to attract extremely talented candidates to the CP residency program.

Dr. Sleckman continued his leadership of the division in the second decade of the 21st Century and appointed Dr. Charles S. Eby as Associate Division Chief for clinical affairs in 2011.
Clinical faculty within the division were spending considerable time helping design and plan space for the new, state of the art, spacious Barnes-Jewish Hospital clinical laboratories that would be located in the newly constructed BJC Institute of Health building, which would be the first physical move for the clinical laboratories since 1974.
The fully automated core lab, automated microbiology and spacious molecular diagnostic laboratories were among the best hospital labs in the country in 2016 and remain so to date.
Another major clinical activity that Dr. Eby oversaw was the division’s role in the standardization of clinical laboratories at all 14 BJC hospitals. While founded in 1996, each BJC institution operated independently until 2015, when BJC leadership mandated standardization for many processes including the clinical laboratories.
Division faculty have played major roles in standardization on a system-wide basis, and as of 2019, ~90 percent of lab testing has been standardized across the system.
Following Dr. Sleckman’s departure 2015, Drs. Eby and Thad Stappenbeck, MD, PhD were named co-chiefs of the division in May 2016 with Dr. Stappenbeck responsible for research activities and Dr. Eby for clinical duties.
Dr. Stappenbeck continued supporting the rich research tradition helped secure division NIH funding that today ranks in the top 20 for all pathology departments nationwide.
In November 2017, two clinical laboratories, Cytogenetics & Molecular Pathology Laboratory and Genomics and Pathology Services (GPS) were combined to form the Clinical and Translational Genomics (CaTG) laboratory. The Clinical Genomics Laboratory performs an array of genetic testing on patient specimens, ranging from traditional cytogenetics to next-generation sequencing and continues to reflect the growing role of molecular techniques in precision medicine today and in the future.
Successful trainees
In August 2017, Laboratory Medical Directors at St. Louis Children’s hospital joined the division, which enriched the experience of trainees by providing direct exposure and supervision in a pediatric lab medicine setting.
Over 95 percent of the trainees from the division have remained in laboratory medicine/pathology during their careers and have had (or are beginning) very successful and recognized careers.
The division has trained a total of 118 clinical pathology residents, including:
- 71 currently in (or retired from) academic positions
- 18 in hospital practice
- 12 in industry
- 9 currently in training
Of the 99 clinical chemistry fellows:
- 50 are currently in (or retired from) academic positions
- 25 are in industry
- 12 are in hospital/private practice
- 9 are in reference laboratories
Of the 16 microbiology fellows trained since 2001, 15 are in academic positions and one is in public health.
Particularly notable are trainees who went on to leadership positions.
- Mike Creer, MD; Penn State Medical Center
- Vishva Dixit, MD, Vice President of Research, Genentech
- Eric Green, MD, PhD; Director, National Human Genome Research Institute (NIH)
- Mike Laposata, MD, PhD; University of Texas Medical Branch (UTMB), Galveston
- John Lowe, MD, PhD; Case Western Reserve
- Jay McDonald, MD; University of Alabama
- Sam Santoro, MD, PhD; Vanderbilt University
- Bryan Wolf, MD, PhD; Children’s Hospital-University of Pennsylvania
- Pampee Young, MD, Chief Medical Officer, American Red Cross
- Sarki A. Abdulkadir, MD, PhD, Vice Chair, Northwestern
- Fred Apple, PhD, Head of Clinical Laboratories, Hennepin County, Minnesota
- Charles Eby, MD, Division Chief, Interim Chair, Washington University
- James Gorham, MD, PhD, Clinical Pathology, University of Virginia
- Robin Lorenz, MD, PhD, Director Pathology Research, Genentech
- Eric D. Spitzer, MD, PhD; Director of Clinical Laboratories and Vice Chair for Clinical Pathology at Stony Brook University
- Xinglong Zheng, MD, PhD, Vice Chair, Clinical Pathology, University of Alabama
Academy of Clinical Laboratory Physicians and Scientists – President
- 1987 – Jay McDonald
- 1995 – Jack Ladenson
- 1997 – Mike Laposata
- 2003 – Fred Apple
- 2004 – David Bruns
- 2005 – David Sacks
- 2009 – Mitchell Scott
- 2012 – Eric D. Spitzer
- 2013 – Robina Lorenz
- 2019 – Stacey Klutts
American Association of Blood Banks – President
- 1982 – Lawrence Sherman
American Association for Clinical Chemistry – President
- 1986 – Jack Ladenson
- 2005 – Mitchell Scott
- 2011 – Ann Gronowski
- 2018 – Dennis Dietzen
American Society for Histocompatibility and Immunogenetics – President
- 1982 – Glen Rodey
Association for Molecular Pathology – President
- 2006 – Barbara Zehnbauer
International Society for Laboratory Hematology – President
- 2011-2014 – Charles Eby