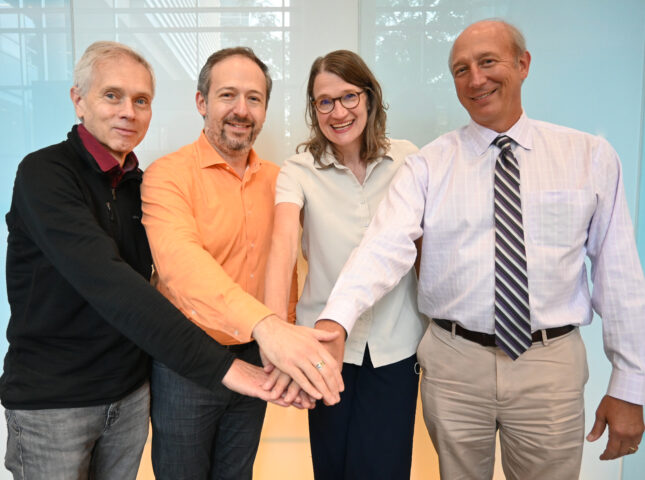
Three faculty members in the Department of Pathology & Immunology at Washington University School of Medicine were recently awarded a multi-year, multi-million dollar grant to research the aging brain. The group, which comprises Jonathan Kipnis, PhD, BJC Investigator, Alan A. and Edith L. Wolff Distinguished Professor of Pathology and Immunology; Gwen Randolph, PhD, Emil R. Unanue Distinguished Professor of Pathology and Immunology; Marco Colonna, MD, Robert Rock Belliveau Professor of Pathology and Immunology; and David Holtzman, MD, Barbara Burton and Reuben M. Morriss III Distinguished Professor of Neurology, has received $15 million over five years from NIH for their project, “Neuroimmunology of AD and CAA with focus on innate immunity and lymphatics.”
“This was a first-time application, which for this type of grant are almost never funded, a testament and recognition of the outstanding group of investigators that have come together to address one of the pre-eminent problems of our time, the aging brain,” said Richard Cote, MD, Professor and Chair, Department of Pathology & Immunology.
The team’s NIH-funded research focuses on myeloid cells including microglia and macrophages and lymphatics in Alzheimer’s disease (AD) and Cerebral amyloid angiopathy (CAA). For years, AD has been studied from the perspective of neurons, amyloid plaques, and tau pathology. In the last decade, researchers have also started to look at glial cells in the brain. Most recently, scientists have examined the interaction between the immune system and AD in disease development. The WashU Med team is looking at peripheral immune cells in addition to microglia and macrophages to see how they might play a role in the development and progression of AD and CAA.
“We’re addressing an emerging area of neurobiology and neuroimmunology. Our research potentially has a big impact for understanding brain biology and in particular, the brain’s immune system,” Dr. Colonna said. “We put together a team of leading researchers involved in macrophage biology, cerebrospinal fluid physiology, and Alzheimer’s disease. We’re among the best experts in the world to tackle this together.”
Each researcher brings different perspectives and strengths to the table; Dr. Randolph is a leading scientist in myeloid cells, lymphatic transport, and lipoprotein trafficking, Dr. Colonna is an expert in microglia, Dr. Holtzman is an expert in Alzheimer’s and other neurodegenerative diseases, and Dr. Kipnis is a leading expert in neuroimmunology, meningeal immunity and lymphatic biology.
“WashU has been a powerhouse in immunology and neuroscience research for decades, so it was natural for us to marry these two disciplines in a strong neuroimmunology collaboration. It is amazing privilege to work with these outstanding scientists and tackle the neuroimmune aspects of Alzheimer’s disease and of cerebral amyloid angiopathy,” Dr. Kipnis said.
The recent NIH funding moves the group forward as they continue to tackle the project. Eventually, the team’s findings could be used to develop genetic, surgical, or pharmaceutical treatments for Alzheimer’s disease.
“We may not be able to replace the dead neurons or directly repair the damaged vessels, but we have numerous ways to target the immune system. I believe that through these immune manipulations, we may be able to delay an onset of Alzheimer’s and ameliorate or slowdown an ongoing disease,” Dr. Kipnis said.